
It is a rare but confronting situation where a pre-hospital and retrieval medicine team are presented with a sick newborn. At one of our recent education days we heard Dr Mark Russell and Dr Mark Newcombe deliver excellent presentations of cases which they had been involved in, involving resuscitative hysterotomy and neonatal resuscitation respectively. Both of these cases reflect some of the high acuity, low occurence scenarios which our teams are prepared to respond to. As a pre-hospital and retrieval service, it’s rare for us to even be around in the first few minutes of a baby’s life, but as our colleagues described, not impossible. So, we took the opportunity to review some of the key issues and processes involved in Neonatal Life Support (NLS) and how we can deliver this using the equipment in our packs.
The newborn in a nutshell
Let’s start with some basics. To those working regularly in neonatology the peculiarities of neonatal physiology will seem second nature. For the rest of us, it is worth spending a moment to revise these as it’ll help to focus on the key interventions needed to resuscitate a newborn.
Airway
The neonatal airway is small, and easily compressible. A large occiput naturally flexes the head and neck unless a small shoulder roll is placed (in contrast to the positioning for older children and adults). It sounds unlikely but babies actually should not have particularly difficult airways (aside from the presence of other syndromes or sequences, for example Pierre Robin).. so long as you know how to manage a baby airway. Like so many skills, it’s easy when you know how, the hard thing is getting the practise. More on airway skills later.
The nutshell: Aim for neutral positioning with a shoulder roll and take care not to compress soft tissues
Breathing
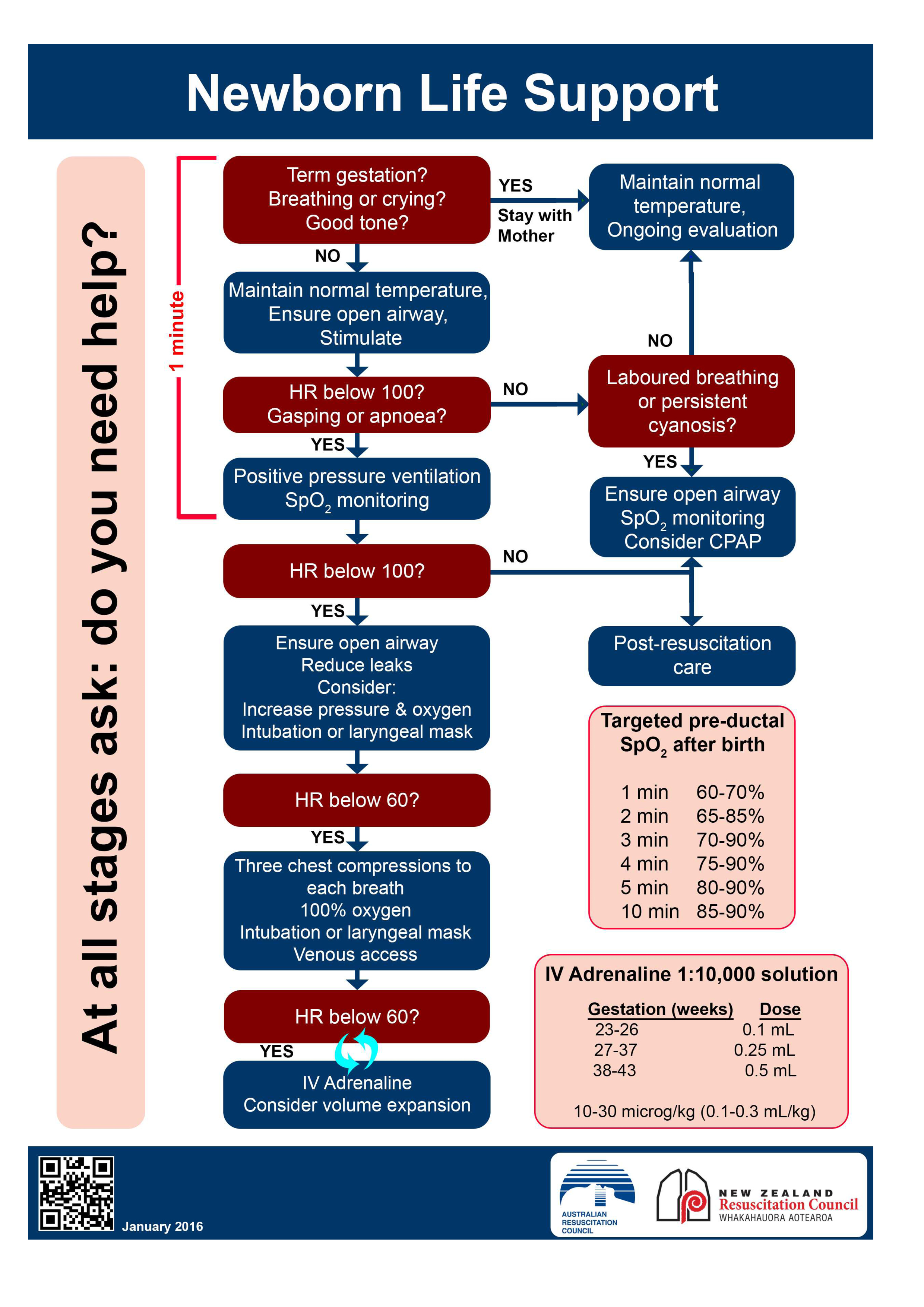
The first breath and cry at birth initiates a series of physiological changes which switch a baby’s circulation from one where oxygenation takes place at the placenta, to one where the lungs are now inflated and responsible for gas exchange. The pulmonary vascular system which is high resistance in utero, now switches to a low resistance system causing the foramen ovale to shut almost immediately at the first cry. The ductus arteriosus follows shortly after, within around six hours, closing off the communication between the aorta and pulmonary artery. It takes a little while for the sats to normalise – use the guide printed on the NLS resuscitation chart for comparison – and always use pre-ductal sats (ie from the right hand). High alveolar resistance means you’ll need higher inflation pressures and always use PEEP (think 30 cmH2O PAWP and 5 cmH2O PEEP). While babies rapidly become bradycardic in response to hypoxia, they are also at risk of retinopathy when exposed to high fractions of oxygen, so it is usual to begin resuscitation in air but increase inspired oxygen fraction as further resuscitation is required.
The nutshell: Hypoxia is very poorly tolerated. Resuscitate in air first, and use higher inflation pressures than you would with adults.
Circulation
We’ve discussed some of the circulation changes at birth above, but as ever, there’s more to consider. The heart muscle is relatively immature, and therefore cardiac output is maintained via heart rate. Babies have a relatively high sympathetic tone which contributes to the elevated heart rate with little room to compensate with contractility… and yet they also have plenty of vagal tone which you may discover when attempting laryngoscopy. The Frank Starling response to volume is more fragile than in adults and it’s relatively easy to fluid overload a baby.
The nutshell: Bradycardia is to be considered a bad sign (but is usually best treated by correcting hypoxia!)
Exposure
Babies get cold quickly. Cold babies can become hypoglycaemic, hypoglycaemic babies develop apnoeas and eventually hypoxia. Temperature therefore needs to be proactively managed from birth to avoid that spiral.
The nutshell: Most babies don’t need intervention at birth, and those who do respond to stimulus and warming, with no further help required. Consider skin-to-skin on Mum’s chest to keep an otherwise well baby warm.
Resuscitation toolkit
We used the Australian Resus Council NLS algorithm as the basis of our workshop, given this is most likely to be familiar to everyone working in critical care regardless of their base discipline. We also referenced the really excellent NSW Ambulance algorithm found on the app as this has been modified for the pre-hospital environment. For those working in NSW ambulance it is worth having the NSWA app on your phone, and the NLS algorithm is easy to find under maternal emergencies (Protocol OP4).
NLS algorithm
NSWA algorithm

Preparing for your resuscitation
- You may have two patients on your hands, if Mum is unwell in any way. This presents an additional challenge in terms of resource management – recruit extra hands early, and consider the need for a second medical team.
- Don’t forget that every ambulance has a maternity kit with bunny rugs, surgical gown, umbilical cord clamps, nappy, tiny warm hat…
- Consider reducing the risk of hypothermia by working inside the ambulance, and warming the vehicle, particularly in winter.
- You may also consider using the warming blanket from the red pack as an under-body warmer, placing this underneath your resuscitation area and then a bunny rug on top to minimise contact with the warming units.
Baby is born, now what…
Start a timer at birth, this will help you keep track of baby’s trajectory. If you have additional hands, delegate a team member to time-keep and scribe.
Warm and stimulate – use a dry towel to rub baby down then change the towel for a clean one or a clean bunny rug. This will take around a minute and often is the most intervention that is required!
Note: a premature baby <32/40 should not be dried – placing the baby into the polyurethane bag so that just head is exposed will help to avoid hypothermia for these babies. Dry their head with a towel which will provide tactile stimulus, and ensure to place a hat if available.
Open the airway – neutral positioning, consider a shoulder roll, avoid compressing soft structures.
Suction – this is a source of constant debate, relating to the risk of aspiration in a baby who is born with significant meconium staining. If baby is already crying, then suction is unlikely to be beneficial. An obtunded baby who has obviously heavy meconium in the airway may benefit from soft suction (use a Y sucker rather than the DuCanto we carry!).
First assessment
Your initial assessment will be based on tone, colour, respiratory effort and heart rate, commonly expressed as an APGAR score (see table). Some tips…
- Use the brachial artery or the umbilicus to feel for a pulse; femoral artery is also a useful pulse point in neonates.
- The APGAR is useful for handing over later on, but try to avoid being distracted by calculating the APGAR if the baby in front of you clearly needs to be resuscitated
- It is extremely unlikely that even the healthiest baby will score an APGAR of 10 at the first minute!
- If baby is crying, pink, vigorous and has a good heart rate >100 then wrap them up warm with a hat and pass to Mum, your work is done…
| 0 | 1 | 2 | |
| Appearance | Cyanotic, pale | Dusky cyanotic peripheries | Pink |
| Pulse | HR < 60 | HR 60-100 | HR >100 |
| Grimace | No response to stimulus | Feeble cry or grimace to simulus | Crying |
| Activity | Floppy | Limited flexion | Flexing, resisting extension |
| Respiratory Effort | Apnoea | Poor effort | Strong cry |
Baby doesn’t look great, now what?
If baby has an increased work of breathing or poor respiratory effort, poor colour, poor tone and/or has a heart rate of <100 then your next step should be to provide ventilatory support.
IPPV
Use the round facemask, attach a PEEP valve at 5 cmH2O. Resuscitate in air in the first instance, and reassess at 30 seconds. Be meticulous with your airway management and ensure you are achieving good inflation. Chest rise is the best guide. If the heart rate has not improved after 30s then increase O2 to 100% and attempt further ventilation.
Reassess again after another 30s.
HR <60
If the heart rate drops below 60 then this is an indication to start CPR. One rescuer should use two hands encircling the baby’s torso with thumbs to provide chest compressions, with a ratio of one breath to three compressions. A secured endotracheal tube may help you to provide more effective ventilation, so it is worth attempting intubation. Be mindful to avoid task fixation, however, and consider an adjunct like an LMA (size 0 carried by regular ambulances) if intubation is difficult.
Remember: fixing hypoxia is the most effective intervention.
Intubating babies
It sounds silly to say, but everything is small. Your movements with the laryngoscope should therefore also be small. Traditional teaching is to use a miller 0 blade in the neonate, but in reality it would make sense to use the technique you are most familiar with (usually a mac blade unless you’re a paediatric anaesthetist).
- Expect the epiglottis to be long and floppy, so you are more likely to get a controllable view if you pick it up with the laryngoscope.
- If using a miller blade, aim to get the tip into the oesophageal inlet then very slowly withdraw the blade until the glottis drops into view (remember, micromovements are the key!).
- Use ELM to assist you, and consider using a stylet in the ETT to aid your control.
- Avoid task fixation, monitor SpO2 during your laryngoscopy attempt and consider using an LMA #0 if you are not able to intubate
- Once intubated, be aware that the tiny, soft tube is easily bent and kinked. Use tape to secure it, and ensure it doesn’t coil up within the mouth, making extubation more likely.
- Always consider siting an NGT in the intubated child, as decompressing the stomach will reduce splinting of the diaphragm. Any amount of pre-intubation crying or positive pressure ventilation massively increases the risk of this.
Reassess at 45-60s
If the HR has improved to >100, maintain ventilation, keep baby warm and move towards hospital. Place a sats probe on the right hand. Consider switching to air if significant improvement in sats and APGARs.
If the HR is 60-100, maintain ventilation, keep baby warm and move towards hospital, place a sats probe on the right hand, continue oxygenation at 100% until HR improves. Reassess progress every 30s.
If HR <60 continue chest compressions. Secure IV access, give adrenaline, consider IV fluid bolus (10mL/kg).
IV access
Your options:
24g IV to dorsum of the hand or the long saphenous vein. This is likely to be difficult in a shocked baby.
IO access: The smallest needle we carry is likely to be quite large for a neonate.
UVC: Our 20g femoral arterial lines (interhospital pack, IV access pouch) could be of sufficient gauge and length for umbilical access, ensure it is flushed with saline prior to insertion. Clean with betadine (blue bag, red loaf) and cut the cord, leaving plenty of length for hospital teams to re-access the umbilicus where possible. The large, compressible, single venous lumen (rather than the two smaller, muscular arterial openings) should accommodate the line. Using sterile gloves, advance until you achieve flashback, use an endotracheal tube tie around the umbilicus to secure in place. Manage the line as you would a central line, and ensure that it is handed over to hospital staff as a pre-hospital UVC.
Adrenaline
IV: 10 mcg/kg (or 0.1-0.3 mL/kg of 1:10,000 adrenaline, eg 0.5mL in a term baby).
ETT: 50-100 mcg/kg (or 0.5 – 1mL/kg of 1:10,000 adrenaline) via ETT if IV/IO/UVC access unattainable
Fluids
It is unusual for babies to be hypovolaemic as a primary cause of arrest, but a fluid bolus of crystalloid 10 mL/kg may be attempted at this stage. Where there is a history of antepartum blood loss, consider giving blood 10 mL/kg. The easiest way to do this in both instances is using a 50mL syringe (interhospital pack, side pocket).
Human factors
Managing a neonatal arrest is challenging on every level, and is not comfortable territory for anyone regardless of your experience or speciality background. It is extremely unusual for a neonate to arrest, and therefore constitutes a massively stressful event for anyone involved. Role allocation and teamwork will help to keep this under control – if you have enough team members, consider allocating a team member to read the algorithm and act as scribe, allocate another team member to draw up drugs, and consider calling for clinical support from the DRC. ACC can also source support from a NETS consultant for you via teleconference (bear in mind this may consume additional bandwidth though).
Post-event
As ever with a case like this, it is important to recognise and acknowledge the emotional fallout which can follow. Look out for yourself, and look out for your colleagues and use the avenues available to you to seek support, be it family and friends, colleagues, or via the employee support services.
ReferencesKariuki, E. et al. (2021) Neonatal resuscitation: current evidence and guidelines. BJA Education. 21 : 12, 470-485. Doi: https://doi.org/10.1016/j.bjae.2021.07.008
This post covers section 1.2.13 of the DipPHRM curriculum.

