Frontotemporal dementia (FTD) is the third most common dementia across all age groups and the leading type of early-onset dementia. This type affects primarily the frontal and temporal lobes of the brain, with a characteristic pattern of atrophy (brain parenchymal loss) on imaging studies. There are two main subtypes of FTD, Behavioural variant (bvFTD) and Primary progressive aphasia (PPA), with the latter being subdivided into non-fluent/agrammatic and semantic variants. The clinical features, aetiology, investigations and management for FTD variants will be discussed below.
FTD was first described by Psychiatrist Dr Arnold Pick between 1892-1906, and the behavioural variant was named after him in 1922. He described the progressive aphasic variant, with associated left temporal atrophy at post-mortem, as well as the behavioural variant being associated with frontal lobe atrophy. Interestingly, the ‘Pick Bodies’, now known to be intracellular tau protein were first described by Dr Alois Alzheimer in 1911. Dr Arnold Pick also trained in Berlin alongside Dr Karl Friedrich Otto Westphal, a fellow psychiatrist who first described the Edinger-Westphal nucleus with Dr Ludwig Edinger.
Contents
- Epidemiology
- Presenting Features
- Frontotemporal dementia subtypes
- The common presenting features
- Behavioural variant (bvFTD)
- Primary progressive aphasia (PPA)
- Semantic dementia
- What are the alternative diagnoses to consider?
- Examination
- Investigations
- Imaging findings
- Diagnosis
- Management
- Take-home messages
- References
- Additional resources
Epidemiology
-The age at presentation typically ranges between 45-65 years and is the most common early presenting dementia. The age of onset is typically earlier than the most common form of dementia, Alzheimer’s Dementia.
-Equal distribution between males and females.
-A positive family history is found in up to 40% of individuals diagnosed with FTD
-Monogenic disease associations, e.g. C9orf72 in Northern Europeans, MAPT, GRN.
Presenting Features
Frontal lobe disease can cause a wide range of symptoms that can affect an individual’s behaviour, personality, and cognitive function. The frontal lobe is responsible for various cognitive processes, including attention, problem-solving, decision-making, planning, and social behaviour. The temporal lobes are broadly involved in the production and understanding of language, recognition of visual stimuli, visual memory recall, appetite control and emotional processing.
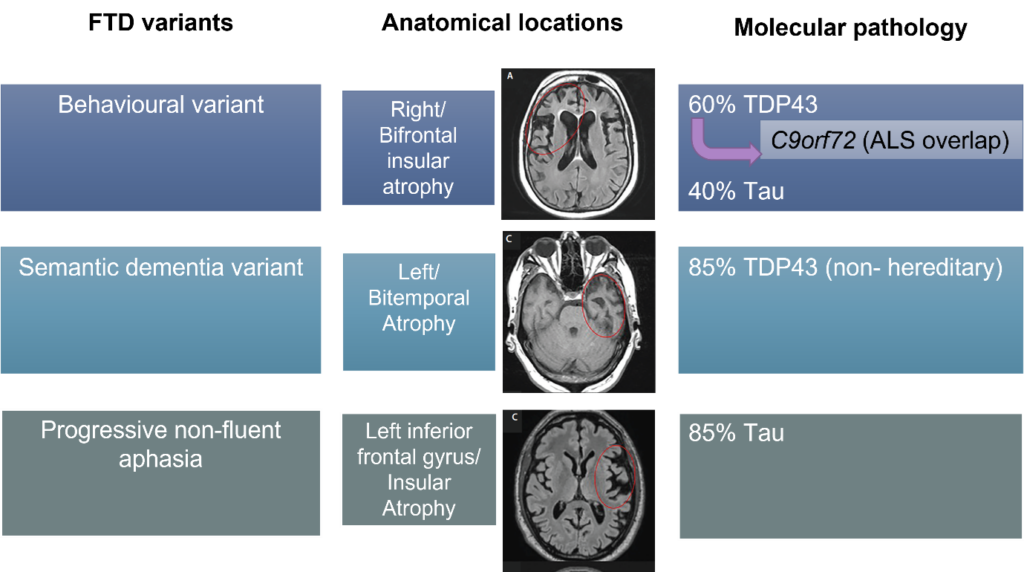
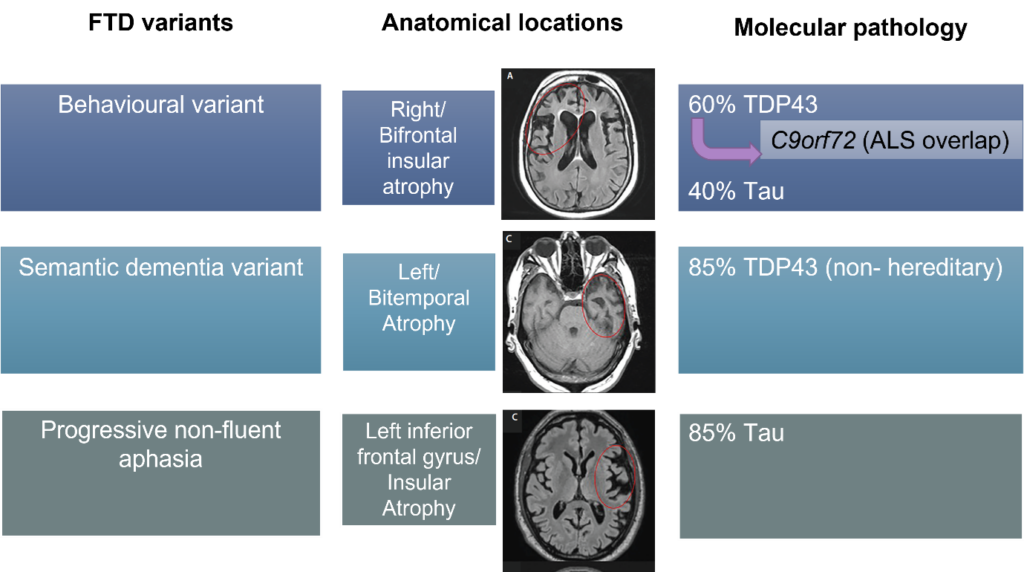
Particular anatomical regions are affected by each variant, which correlates to the clinical presentation and the specific causative molecular pathology. Over time with progression of the disease the clinical features overlap between variants as other brain areas become involved.
Frontotemporal dementia subtypes


The common presenting features


Behavioural variant (bvFTD)
The prominent initial features are chronic alterations and deterioration in personality, social functioning and behaviour. The pathological changes originate from the orbital and medial frontal lobes, typically on the right side of the brain. The presenting features are listed above in the above table. The molecular mechanism behind this variant includes tau pathology (overlap with parkinsonian disorders, such as progressive supranuclear palsy and corticobasal degeneration) or TDP43, a gene involved in the regulation of gene expression in neurons.
The behavioural variant of FTD has a known association with ALS given a common pathological genetic process, which is inherited in an autosomal dominant pattern. Percentage concurrence.
Pathological expansions in the gene C9orf72 are responsible for 40-50% of familial ALS cases, 30% of familial FTD and up to 21% of sporadic cases of FTD. It is a hexanucleotide repeat expansion (GGGGCC), with the normal number of repeats in the region of 20-30, whereas pathological repeats are usually over 100. Approximately 15% of those with FTD have it with ALS, and approximately 25% of ALS patients have FTD.


Diagram outlining the relationship between the clinical syndromes of bv-FTLD and ALS, either can be present in isolation, but they can co-occur or develop in succession.
Primary progressive aphasia (PPA)
In this variant, prominent language impairment is an early feature with word-finding difficulty, inability to recall everyday objects (anomia), repetition of words others say (echolalia) and motor speech impairment (apraxia). The other name for this is non-fluent aphasia. People with PPA typically understand the meaning of words and can recognise the object in front of them but have difficulty with name recall and articulation. In addition to speech apraxia, they can also be found to have orobuccal apraxia on examination, which is the inability to cough or yawn on command.
Some textbooks and articles will discuss the variant logopenic aphasia, which is now recognised as a presentation of Alzheimer’s disease rather than FTD, where individuals have word-finding difficulty, with intact semantic understanding and absence of motor speech impairment (apraxia).
Semantic dementia
People with semantic dementia exhibit early loss of the meaning of conceptual knowledge, such as the meaning of words, and the ability to understand facial expressions or objects. They may often ask what a word means or what an object does. They may exhibit avoidance in naming objects, but grammar remains intact. In the Montreal Cognitive Assessment (MoCA) for example, instead of correctly naming the zebra, they may instead call it a ‘horse’ or an ‘animal’. Mispronunciation of words, such as ‘pint’ may also be noted. Individuals with this variant of FTD also subsequently develop behavioural features, like bv-FTD.
What are the alternative diagnoses to consider?
It is worthwhile to have an open mind with these presentations, as cognitive decline and changes in behaviour can have a multitude of causes. There is considerable overlap in symptoms across different types of dementia, posing diagnostic challenge. As with any suspected dementia, it is also important to rule out potentially reversible causes, especially in young patients where there is a wider net including rarer disorders. A younger patient with suspected dementia should raise suspicion of a genetic cause. It is important to do a prompt referral to a neurologist with the completion of suitable investigations. It may be that the patient does not have FTD, but instead another disorder, such as those listed below.


Examination
On examination, you may note primitive reflexes e.g. grasping, evidence of self-neglect, and obesity secondary to hyperphagia.
Bulbar muscle weakness, muscle wasting, and fasciculation may indicate the FTD/MND crossover syndrome.
Investigations
-CT/MRI head illustrates in FTD, prominent frontal or temporal lobe atrophy, at the latter stages of atrophy being classic ‘knife edge gyri’ and deep widened sulci.
-Montreal Cognitive Assessment (MoCA)/ Addenbrooke’s cognitive assessment (ACE)/ Frontal assessment battery (FAB) illustrating deficits in attention, semantic memory or articulation.
-The Mini-mental state examination (MMSE) is not sensitive to this dementia, so alternative tests should be conducted as above.
-A specialist may subsequently investigate for genetic causes of dementia, particularly for this subtype of dementia as there are a number of recognised pathogenic variants.
Imaging findings
Particular anatomical regions are affected by each variant, which correlates to the clinical presentation and the specific causative molecular pathology.
The textbook appearance of severe frontotemporal disease in FTD is so-called knife-edged gyri with deep widened sulci.
Diagnosis
The diagnosis for any dementia is primarily a clinical one. This is from a comprehensive history with often a collateral history from a relative, and performance on appropriate cognitive testing. A full neurological examination should also be undertaken to evaluate for other causes of cognitive decline or to look for features of an ALS overlap syndrome.
There are diagnostic criteria for the FTD subtypes, and in the references these criteria are linked. They include inclusion criteria of the classical history findings and cognitive testing patterns.
Of those with FTD, 40% have a positive family history. In these cases, particular genetic testing is offered for the patient and close family members to ascertain the mode of inheritance and for prognostic and therapeutic value. 90% of cases found to be genetic are due to mutations in the MAPT, C9orf72 and GRN genes.
Most patients will undergo either CT or MRI brain imaging also, which together with the clinical history and examination can assist with staging and prognostication of the disease, as well as rule out an additional intracerebral pathology.
Gold-standard:
The only confirmatory study for dementia is histology, which is typically taken post-mortem, and in the case of FTD typically illustrates cortical and subcortical gliosis, with or without intracellular tau inclusion bodies. This is not usually conducted given the diagnosis being made based on the history and investigation findings.
Management
The big focus of management is reducing risk. These patients are impulsive and can be at high risk of accidental injury, aggression, and self-neglect. Removal of access to driving is a common discussion as these patients typically present at younger ages without physical frailty.
Psychological support for caregivers is also key, as the behaviours and needs of these patients have a high burden and impact on their relatives. Input from physiotherapists, occupational therapists and psychologists is necessary to evaluate the modifications needed to the home of patients and their relatives and the need for supported living. Support from specific agencies, such as the Rare Dementia Support group (www.raredementiasupport.org) may be beneficial.
The impulsivity, aggression and agitation may indicate the need for medications, such as antipsychotics. Please see our psychiatry page for useful resources regarding psychotropic medications for Behavioural and Psychological Symptoms of Dementia (BPSD) and antipsychotics in the Older Adult population.
Take-home messages
– There is a high rate of carer burden with this form of dementia given the alterations to personality and social functioning of these individuals.
-Often the collateral history is one of the most valuable tools for the diagnosis of frontotemporal dementia.
-An MMSE is not sensitive to this form of dementia, so other cognitive assessments should be utilised (FAB, ACEiii, MoCA)
-The initial presentation correlates to specific anatomical regions that are involved, with overtime the subtypes clinically converging due to extensive/ generalised atrophy of the frontal and temporal lobes
-This form is often familial; therefore, referral of first-degree relatives for genetic counselling and testing should be offered for future family planning.
-The gold standard diagnostic test is brain histology at post-mortem, but this is rarely carried out.
References
Journal articles:
Bang J, Spina S, Miller BL. Frontotemporal dementia. Lancet. 2015 Oct 24;386(10004):1672-82. doi: 10.1016/S0140-6736(15)00461-4. PMID: 26595641; PMCID: PMC5970949.
Boeve BF, Boxer AL, Kumfor F, Pijnenburg Y, Rohrer JD. Advances and controversies in frontotemporal dementia: diagnosis, biomarkers, and therapeutic considerations. Lancet Neurol. 2022 Mar;21(3):258-272. doi: 10.1016/S1474-4422(21)00341-0. PMID: 35182511.
Rascovsky K, Hodges JR, Knopman D, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134(Pt 9):2456–2477. Provides the new framework for the classification and diagnosis of behavioral variant FTD (bvFTD)
Websites:
Practical Neurology- Frontotemporal dementias
Medlineplus- C9orf72
Textbooks:
Oxford Textbook of Medicine, Chapter 24.15 The motor neuron diseases, Tom Jenkins, Alice Brockington and Pamela J- Shaw.
Oxford Textbook of Medicine, Chapter 24.4.2 Alzheimer’s disease and other dementias.
Additional resources
Books:
What I wish people knew about dementia, from someone who knows- Wendy Mitchell 2022.
A personal account of being diagnosed with dementia at a young age.
Podcast episodes:
The Brain Health Revolution Podcast– ‘Bruce Willis and his battle with Aphasia’ April 2022
A broader discussion of the causes of aphasia, but also focussing on FTD, which Bruce Willis has later been diagnosed with.
All In The Mind– ‘Utterly catastrophic- life with frontotemporal dementia’ February 2022
Interview with the partner of an individual with FTD, with a discussion of presentation and carer impact. Also interviewed is the Frontier Chair Professor Olivier Piguet, a research group on FTLD.
Navigating Neuropsychology– 84 Behavioural variant frontotemporal dementia – with Dr Bruce Miller. A more focused and extensive discussion related to neuropathology overlaps with other neurodegenerative disorders and diagnostic criteria of the different subtypes.
This article was written by Dr Isobel Platt (FY2 Neurology), edited by Professor Gabriele De Luca (Consultant Neurologist) and Dr Jacob Day (Neurology SpR)
How useful was this post?
Click on a star to rate it!
Average rating 4.5 / 5. Vote count: 2
No votes so far! Be the first to rate this post.
We are sorry that this post was not useful for you!
Let us improve this post!
Tell us how we can improve this post?



