Abortion history in Canada is Complex. Countless hardships were overcome on the long journey to the legalization of medical induced abortion (IA). This blog post will focus on what you need to know as an acute care provider.
Context:
Unsafe abortions are the leading preventable causes of maternal death and morbidity (4.7-13.2% of maternal deaths). They lead to significant health costs associated with complications and loss of income from long-term disability. Barriers to safe induced abortions are worsened by stigmatization, with restrictions violating the human rights of women and pregnant people including their right to privacy, non-discrimination, and equality
- Medical abortions are common
- 50% of pregnancies worldwide are unintended
- 60% of all unintended pregnancies and 30% of all pregnancies end in induced abortion
- 45% of all abortions are unsafe, of which 97% take place in developing countries.
- In Canada, 31% of Canadian women undergo an abortion during their reproductive lifespan and abortions are the 2nd most common reproductive health procedure (SOGC, 2016)
- Changes since the approval of Mifegymiso as a medical abortion regimen:
- In countries where MIFEGYMISO was approved, the overall abortion rate has remained stable but the rate of medical abortions has increased.
- The percentage of medical IA compared to total IA increased from 2.2% to 31.4% since Health Canada authorized Mifegymiso.
- Medical abortions facilitate access in geographic areas where surgical access is challenging
- Lack of access to medical abortions is problematic:
- A 2019 CJEM study group showed that patients experiencing complications of early pregnancy often present to EDs and most do not have an established obstetrical provider. They surveyed 71 EDs in Ontario, 63 responded. Of those who responded, 54% did not have access to early pregnancy clinic services for women who presented to ED with early pregnancy complications.
What is a Medical Abortion (MA)?
- Induced abortions include both medical and surgical options
- A medical-induced abortion is a process in which a pregnancy is voluntarily interrupted through the administration of medications.
- Since its approval by Health Canada in 2015, most medical abortions are completed with Mifegymiso
- What is Mifegymiso?
- A combination of mifepristone and misoprostol for medical abortions
- Mifepristone: Anti-glucocorticoid or a cortisol receptor blocker; an antiprogestin that prepares the uterus for misoprostol. It has been shown to shorten the interval of action and effectiveness of misoprostol.
- The mifegymiso kit contains 200mg of oral mifepristone
- Misoprostol: Prostaglandin that causes cervical ripening and augments uterine contractions.
- The dose is 800mcg – four 200 mcg tablets which can be taken orally, sublingually, or vaginally.

A Stepwise Approach to Medical Abortions in the ED
Step 1: Review Indications/Contraindications
Indications: Unintended pregnancy
- For unintended pregnancies, it is important that the patient has capacity and provides informed consent.
- The patient must have a confirmed pregnancy (by urine or serum beta HCG).
- Mifegymiso is used for pregnancy up to 49 days of gestation but robust data supports its use as an effective regimen up to 70 days.
- Given that effectiveness drops after 64 days of gestation as per the National abortion federation, in the ED, <64 days will probably be within our comfort zone. We will review the modified regimen after 64 days. Of note, there is no absolute lower gestational age limit.
Indications: Intended pregnancy with abnormalities
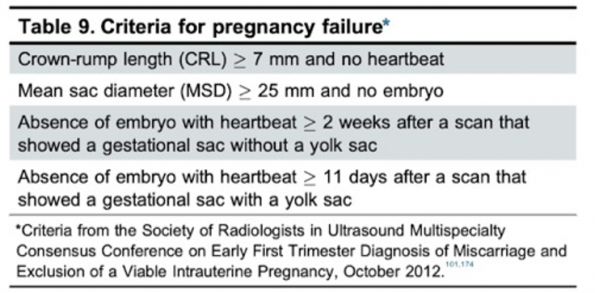
- Indications for an intended pregnancy with abnormalities are difficult to establish in the ED as it refers most often to first-trimester pregnancy loss
- There are specific pregnancy failure criterion that needs to be met. We may have this information if the patient has obtained a radiology performed ultrasound however this is not frequently the case in the ED.
- The ultrasound report would include a mention of “fetal demise” or “pregnancy failure” and may include specific criteria such as the absence of fetal growth, absence of fetal heartbeat or empty gestational sac.
Contraindications to medical abortion
- Patient ambivalence or lack of informed consent
- There is a risk of teratogenicity with misoprostol and low risk with mifepristone. Therefore, the pregnant patient should be certain of their decision.
- Unconfirmed or unreliable gestational age
- IUD in place
- Higher likelihood of having an ectopic pregnancy should have an ultrasound to r/o ectopic. If intrauterine pregnancy (IUP) is confirmed, the IUD should be removed
- Hemorrhagic disorders or anticoagulant therapy
- Oral steroid therapy and adrenal failure – mifepristone is a potent anti-glucocorticoid and may potentially impair the action of cortisol
- Uncontrolled asthma – mifepristone has anti-glucocorticoid effects
- Allergy to medications
Step 2: Counselling
Trauma-Informed Care
- It is important to provide trauma-informed care as this is often a delicate/vulnerable situation for patients. It is important to acknowledge this and provide non-judgemental support.
- Maintain a confidential environment
- Provide options
- Medical and surgical induced abortions are available for first-trimester pregnancies.
- Patients who choose their method of abortion have a higher satisfaction rate.
- If concealment is needed for IA due to social circumstances/risk of safety to the patient, a surgical IA is more definitive with less bleeding and visible side effects.
Symptoms to expect with medical abortion
- Medical abortions are symptomatic
- There will be abdominal cramping and vaginal bleeding which begins approximately 2-4 hours after taking misoprostol
- Other side effects of misoprostol include:
- Low-grade fever
- Dysuria
- Nausea, vomiting and diarrhea
- After 10 weeks of gestation, patients may see the embryo which measures up to 3cm
Breastfeeding/subsequent pregnancies
- Lactation is safe without concern for side effects in infants.
- Patients may become pregnant again at any time after a medical IA however experts suggest waiting until next menstrual cycle to ease tracking of gestational dates.
- Medical IA does not impact fertility, unlike surgical IA which is associated with slightly decreased fertility due to uterine scarring.
Discuss contraception/provide resources
- It is important to discuss contraception with your patient as there is a rapid return to fertility estimated to be within 20 days
- Useful resources to share with your patients include:

Risks of medical abortion include:
- Hemorrhage
- Infection
- Continuing pregnancy with teratogenicity due to medications consumed
- Risk of needing a surgical intervention. The higher the gestational age, the lower the success rate of medical IA.
- The mortality risk associated with medical IA is substantially lower than in pregnancy (<1 in 100 000 (medical IA) vs 10 in 100 000 (pregnancy) in Canada) (SOGC, 2016)
Step 3: Investigations
- Beta HCG
- A serum beta HCG is not necessary if the patient has a good recollection of their last menstrual period and can confirm dates by history
- If dates by history are unknown, obtain a serum beta HCG on initial presentation. This will be required for follow-up
- If dates by history are known, a urine beta HCG is adequate to confirm pregnancy.
- If dates aren’t known and you complete a serum beta HCG, recall that HCG levels peak at 8-10 weeks gestation with values that can range between from 5000-150 000 mlIU/ml but are typically between 60 000-90 000 mlIU/ml. After 8-10 weeks gestation it does become more constant at 12 000 mlIUml.
- CBC
- Only required if there is a risk of bleeding as per medical history and patient symptoms
- Routine hemoglobin and hematocrit have not been shown to improve outcomes in first-trimester abortions
- RH
- Emerging epidemiologic and clinical evidence indicates that the risk of hemorrhage caused by early abortion is negligible and Rh testing and provision of Rh immune globulin may not be necessary
- There is no evidence that providing anti-D immunoglobulin (Rhogam) in early pregnancy prevents alloimmunization and poor outcomes in a subsequent pregnancy. Providers can forego Rh testing and anti-D immune globulin if patients are under 12 weeks from last menstrual period (LMP)
- The SOGC provided a COVID update which stated that the RH is not required for up to 70 days/10 weeks gestation but have not updated formal guidelines for first trimester pregnancies.
- Ultrasound
- Ultrasound is not required for medical IA if there are no risk factors or signs/symptoms of ectopic pregnancy such as previous ectopic pregnancy, tubal surgery, IUD, history of pelvic inflammatory disease and symptoms such as abdominal pain and vaginal bleeding.
- Ultrasound should be reserved for:
- Patients with uncertain pregnancy dating
- Risk factors for ectopic pregnancy
- Symptoms consistent with ectopic pregnancy
- In the ED, patients may present with abdominal pain or vaginal bleeding. Below is a flow diagram with a reasonable approach for ED providers.
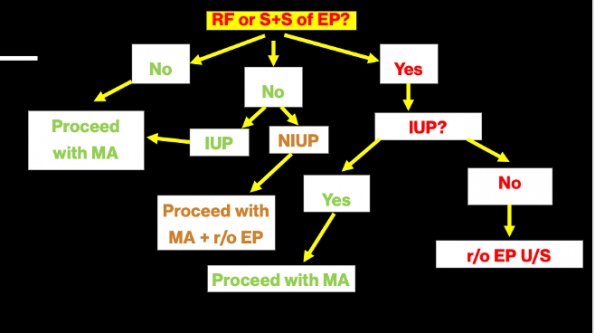 ** Diagram is based on simplified versions of the NAF/SOGC recommendations for pregnancy of unknown location**
** Diagram is based on simplified versions of the NAF/SOGC recommendations for pregnancy of unknown location**
-
-
-
- If your patient does not have risk factors and signs of EP, proceed with MA
- If your patient is at risk of having an EP then proceed with POCUS in the ED to try and confirm IUP
- If IUP: proceed with MA
- If NIUP: you must r/o ectopic if patient is symptomatic with a radiology performed ultrasound. If asymptomatic can proceed with MA (see below-PUL)
- If pregnancy of unknown location (PUL)
- No risk factors/symptoms of EP
- In a patient with a PUL who is requesting MA, they should receive abortion care without delay provided that they have no clinical symptoms of ectopic pregnancy
- Continue the workup to rule out an ectopic pregnancy as MA will not treat an EP and delayed diagnosis may increase complication risks.
- These patients require a radiology-performed ultrasound. If that is not possible, a follow-up beta HCG is required until the EP is excluded and/or the abortion is complete or transfer of care is available.
- Misoprostol acts on smooth muscles and therefore will have not be effective for an ectopic pregnancy. Mifepristone is a synthetic glucocorticoid that acts on progesterone receptors and also will not affect an ectopic pregnancy.
- No risk factors/symptoms of EP
-
-
Step 4: Medical Regimen
Mifegymiso
- <64 days
- Mifepristone
- Can be taken outside of the ED
- Not effective on its own – must be taken in combination with misoprostol
- Misoprostol
- Taken 24-48 hours following mifepristone
- Side effects include moderate to heavy vaginal bleeding within 2-4 hours of medication ingestion, cramping, nausea and vomiting
- Mifepristone
- >64 days – 77 days
-
- Additional regimens are published and routinely utilized by physicians providing abortion care for gestational age >64 days. Most suggestions include an optional or additional dose of misoprostol.
-
Analgesia
- NSAIDs (ie. Ibuprofen) are more effective than acetaminophen for pain control and do not interact with misoprostol
- The risks of narcotic analgesia for pain management may outweigh the benefits.
Effectiveness of medical abortions
- Oral mifepristone and misoprostol is 95-97% effective in the first 49 days after the last LMP (SOGC)
- The NAF guidelines outlines that the effectiveness decreases after 49 days of gestation but remains >90%.
- Patients’ and clinician’s assessments of successful expulsion based on medical history are highly predictive of complete abortion (sensitivity 99.1%, specificity 45.5%). Studies have shown that patients are quite accurate at identifying when they have passed products of conceptions.
- A sign of ongoing pregnancy includes minimal or no bleeding after misoprostol.
- Many studies the compared efficacy of early SA vs MA. A study with >33 0000 SAs and nearly 17 000 MA using MIFEMISO in GA <63 days the ongoing pregnancy rate was slightly higher among women undergoing MA (0.3 vs 0.1%, RR 2.2, P=0.0001). (Bender, 2011)
Step 5: Follow-up Care
- The challenge of follow-up in the ED
- This will ultimately be the rate-limiting step in providing MA in the emergency department
- These patients require follow-up. Return to ED visits are often scheduled for patients in smaller communities and are feasible. That being said, it may be challenging to hand over patient care to physician colleagues who may not be familiar or comfortable with providing medical abortion care.
- Our hope is that with increased awareness and education, this will become more feasible.
- Follow up methods
- If you have obtained a serum beta HCG, these patients can be feasibly followed up in the ED due to rapidly decreasing levels.
- 3-4 days should have a 50% reduction if attained no further follow up
- 7-10 days should have an 80% reduction if attained no further follow up
- A single follow serum beta HCG is all that is needed
- Urine beta testing should not be checked before 4 weeks after abortion.
- At 4 weeks after medical abortion, approximately 20% of patients will have a positive pregnancy test.
- If the patient reports passing clots, cessation of vaginal bleeding, and symptoms of pregnancy, then the medical abortion is also determined to be complete
If none of these above are met, a referral to a local family planning clinic is suggested. This patient may require additional trials of MA or SA.
Step 6: Other Options
Options vary per local and provincial jurisdiction
- Medical IA
- <9 weeks (64 days)
- Standard MA protocol
- 9-11 weeks (64-77 days)
- Modified MA protocol
- <9 weeks (64 days)
- Surgical IA
- <14 weeks
- Dilation and curettage
- 14-24 weeks
- Dilation and evacuation
- >24 weeks
- Feticide injection and induction of labor
- This is offered into the late 3rd trimester but access is limited. There is legally no limitation to this but finding a practitioner is difficult and often at this point social work becomes involved with alternative suggestions such as adoption.
- <14 weeks
Step 7: Awareness of Possible Complications
- Rate of complications
- According to the SOGC, severe complications of MA are rare
- A cohort study published in the Annals of Internal Medicine in 2023 compared 39 856 women dispensed mifepristone-misoprostol as outpatients vs 65 176 women undergoing procedural abortions at 14 weeks of gestation or earlier in outpatient clinics in Ontario between 15-49 years old.
- The primary composite outcomes of any SAE within 42 days after procedural abortion (severe maternal morbidity, EOD, ICU admission, or death).
- 133 women (medical) vs 114 women (procedural) had the primary outcome. ARR of 1.5 per 1000 (CI 1.44-2.43)
- Hemorrhage
- The risk of excessive bleeding after MA is 0.1%. Excessive bleeding is usually secondary to uterine atony and tissue retention.
- Bleeding is expected with medical abortions but should not exceed more than 2 maximum absorption pads in 4 hours
- Management principles are almost identical to those in postpartum hemorrhage.
- Endometritis
- Endometritis is a cause of morbidity in childbearing women. It is an infection of the decidua which is pregnancy endometrium or retained products of conception (RPOC).
- It is a complication of both medical and surgical IA, medical due to retained tissue of conception and surgical due to the procedure itself and introduction of pathogens.
- In medical abortions, it occurs at a rate of approximately 1% when Misoprostol is administered vaginally compared with 0.2% when taken orally or sublingually.
- Endometritis is in the PID spectrum along with salpingitis and Tubo-ovarian abscess (TOA). It is typically a polymicrobial infection
- Lack of early recognition can lead to serious complications like intraabdominal abscess, septic shock, toxic shock syndrome, or necrotizing infections.
- Our goal is early diagnosis and commencement of empiric treatment.
- Common signs and symptoms include:
- Abdominal or pelvic pain
- Foul-smelling vaginal or cervical discharge
- Prolonged vaginal bleeding or spotting
- Fever or chills (more than 24 hours after misoprostol)
- Uterine or adnexal tenderness
- Elevated white blood cell count
- Clinical criteria – 2 of 3 the following:
-
- Fever
- Uterine tenderness
- Purulent uterine discharge
-
- Investigations
-
- Ultrasound
- The changes on ultrasound are nonspecific and overlap with normal changes of pregnancy to the uterus such as gas, fluid and enlargement of the uterus.
- A patient may have RPOC on ultrasound without endometritis and may also have endometritis with a normal ultrasound. However, if there are clinical signs of endometritis, an ultrasound is needed to assess for RPOC which would require surgical removal for source control
- Ultrasound
-
- Common signs and symptoms include:
-
-
- Management of endometritis in the context of IA will vary:
- If the patient underwent a surgical IA, consult OBGYN
- If the patient underwent an MA:
- If the patient has infectious symptoms but is systemically well, they can be discharged home with outpatient antibiotics as long as source control isn’t required.
- Criteria for inpatient treatment are similar to those in PID and include:
- Failed outpatient management
- Source control required
- Complications such as TOA, sepsis
- Antibiotics
- Outpatient management includes Ceftriaxone IM/IV X1, followed by a course of Doxycycline + metronidazole PO
- Inpatient management includes Cefoxitin and doxycycline or clindamycin and gentamicin
- Management of endometritis in the context of IA will vary:
-
- Uterine perforation
- Perforation is a rare (<2%) complication of surgical IA. They are usually recognized in the operating room but there can be a delay to recognition.
- Perforation may be to the fundal or lateral aspect of the uterus.
- Symptoms are secondary to hemorrhage and peritonitis which include diffuse abdominal pain, distension, hematuria and vaginal bleeding.
- Ultrasound may show loops of bowel incarcerated in uterine defect and abdominal free however patients will often require a CT scan to localize the site of perforation
- Consult gynecology for this complication.
- Important to note that fundal perforation is less likely to bleed but more risk of bowel/bladder injuries
- Often treated expectantly with monitoring
- Lateral perforations have more risk of hemorrhage due to the location of uterine arteries.
- The management if laparoscopic exploration
- Important to note that fundal perforation is less likely to bleed but more risk of bowel/bladder injuries
Take home points
- Abortion care is primordial, bridging gaps in a long history of barriers to reproductive rights and access to care
- Abortion care is generally safe and can be a part of your practice in the ED as long as reliable follow-up planning is possible
- Trauma-informed care and counseling is necessary in abortion care
- Complications are rare but important to recognize them rapidly
References