You are seeing your next patient in urgent care, a 35-year-old female with a wrist injury who has been waiting for 6-hours. After sending her for an x-ray and offering pain control in the ED, she tells you she is 3-months post-partum and is currently nursing. She asks if there are any pumps available in the ED for her to use, and if the medication you are giving her is safe for her infant.
In the emergency department, it is quite common to encounter lactating patients; they are either patients themselves, or may be visiting others. In the ED specifically, excessive (unanticipated) wait times, lack of physical space, situational stress, and lack of provider knowledge present unique challenges.
This blog post will review basics of lactation physiology, chestfeeding complications, medication and diagnostic imaging considerations.
Lactation Physiology
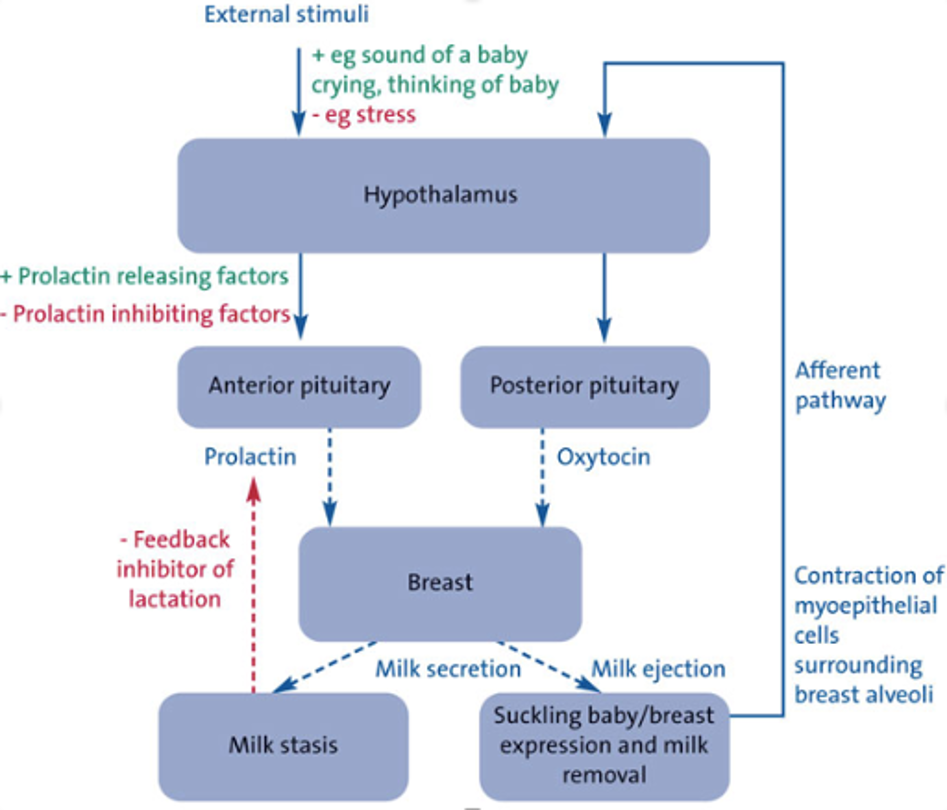
First, it is important to understand the basics of lactation physiology, to better advocate for and support lactating ED patients.
For newborns, it is recommended to feed every 8-12 times/day, with feeding sessions ranging from 5-10 minutes to sometimes up to an hour. Once lactation is established and maintained, production is regulated by a substance that is called feedback inhibitor of lactation (FIL). The role of FIL is to regulate the amount of milk produced based on how much the baby takes (Figure 1). Removing milk removes the inhibitor, and promotes milk secretion. If the milk is not removed, elevated intra-mammary pressure and accumulation of FIL reduce milk production.
Therefore, to ensure adequate supply is maintained, it is important to advocate for infant feeding or to offer breast pumps while patients wait to be seen and treated. Additionally, we must be aware of repercussions when as providers we advise patients to “pump and dump” or to not feed their infant in response to certain treatments or medications provided. This can decrease supply, lead to complications such as mastitis/abscess, and jeopardize a healthy nursing journey between the patient and their infant.
Complications of Lactation
Complications on the “mastitis spectrum” can arise from lactating, which results from ductal inflammation and edema (Figure 2). If ductal narrowing and alveolar congestion are worsened by overstimulation of milk production, inflammatory mastitis can develop. This can then progress into acute bacterial mastitis, a phlegmon, or abscess.
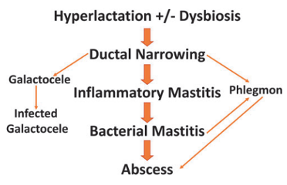
Figure 2. Mastitis spectrum
The Academy of Breastfeeding Medicine revised its guidelines on the mastitis spectrum in 2022 (Table 1 and 2), which includes:
| General Recommendations | Medical Interventions |
|
|
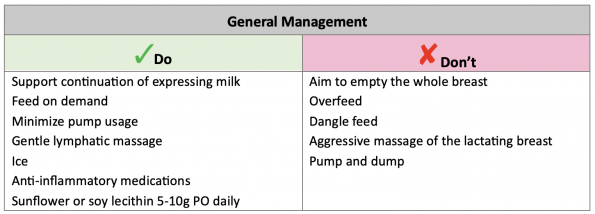
Table 1. General management of mastitis
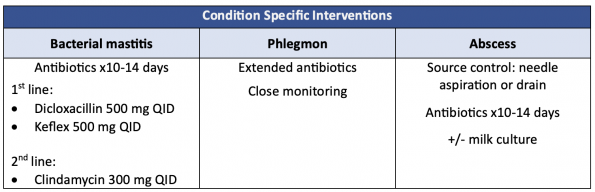
Table 2. Medical management of mastitis
Drugs and diagnostic imaging in lactating patients
Emergency physicians must be comfortable counseling patients regarding medication use and (dis)continuing chestfeeding. The QR code below will guide you to resources you can use as a physician and serve as a patient resource about the safety of drugs in lactating patients.

Figure 3 Lactation resources
Table 3 is a review of commonly used medications in the ED and their safety profile for lactating. However, for any drug, in practice, you can use the LactMed® website.
In general, the safety of drugs in lactating patients is described by the relative infant dose (RID). This is the weight-adjusted percentage of the parental dosage ingested by a fully chestfed infant. An RID of <10% is considered safe, caution is required when the RID is 10-25%, and drugs with an RID of >25% is generally considered not safe.
Table 3. Medications and diagnostic imaging
References
https://sjrhem.ca/tag/pregnancy/
https://www.tamingthesru.com/blog/grand-rounds/recap-080322
https://www.bfmed.org/protocols?fbclid=IwAR2RuEukLmizrUdfHeSC4D0JS9y6KDN7Z3hDB_941V7KbVQLzweXdEvMtDs
https://www.bfmed.org/assets/ABM Protocol %2336.pdf
https://www.bfmed.org/assets/DOCUMENTS/PROTOCOLS/Protocol%20%2331%20-%20English%20Translation.pdf
https://foamcast.org/2018/05/01/emergency-care-of-lactating-patients/



Trackbacks/Pingbacks